Understanding What Happens When You Stop Using Drugs
Drug withdrawal symptoms are the physical, psychological, and emotional effects that occur when a person reduces or stops using a substance their body has become dependent on. These symptoms range from mild discomfort to severe, life-threatening complications depending on the substance, duration of use, and individual health factors.
Common drug withdrawal symptoms include:
| Physical Symptoms | Psychological Symptoms | Severe Risks |
|---|---|---|
| Nausea and vomiting | Anxiety and depression | Seizures (alcohol, benzos) |
| Sweating and chills | Irritability and mood swings | Delirium tremens |
| Muscle aches and pains | Difficulty concentrating | Cardiac complications |
| Tremors or shaking | Hallucinations or paranoia | Dehydration |
| Insomnia and fatigue | Intense cravings | Suicidal thoughts |
Withdrawal timelines vary by substance:
- Alcohol: Symptoms begin 6-24 hours after last drink, peak at 24-72 hours, last 2-10 days
- Opioids: Onset 8-24 hours (short-acting) or 2-4 days (long-acting), duration 4-20 days
- Benzodiazepines: Begin 1-4 days after last use, can last weeks to months
- Stimulants: Start within 24 hours, typically last 3-5 days
Important: Withdrawal from alcohol and benzodiazepines can be life-threatening without medical supervision. If you or a loved one is experiencing withdrawal symptoms, call our 24/7 confidential helpline at 866-720-3784 for immediate guidance.
Withdrawal happens because your brain and body have adapted to the presence of a substance. When you suddenly remove that substance, your body needs time to readjust to functioning without it. This process can be uncomfortable, painful, and in some cases dangerous.
Many people trying to quit describe withdrawal as feeling like a severe flu combined with intense emotional distress. As one medical guideline notes, “Withdrawal management refers to the medical and psychological care of patients who are experiencing withdrawal symptoms as a result of ceasing or reducing use of their drug of dependence.”
The good news? Withdrawal is temporary, and with proper medical support, it can be managed safely.
At Drug Rehab Headquarters, we’ve helped thousands of individuals and families steer drug withdrawal symptoms and find effective treatment options. Our team of addiction specialists understands the challenges of withdrawal and connects people with the resources they need for safe, successful recovery. If you’re struggling with withdrawal or considering getting help, we’re here to guide you through every step of the process—call us at 866-720-3784 anytime.

Have you ever wondered why stopping a daily habit, like that morning coffee, can leave you with a headache? That’s a tiny glimpse into withdrawal. Now, imagine that feeling amplified a hundredfold, affecting your entire body and mind. That’s the reality for someone going through drug withdrawal symptoms.
At its core, drug withdrawal occurs when your body, which has grown accustomed to a drug’s presence, suddenly has to function without it. This isn’t just about willpower; it’s a profound physiological response. When you use certain substances regularly, your brain and body adapt to their continuous presence. This adaptation is called physical dependence. It’s crucial to understand that physical dependence is different from addiction, though they often go hand-in-hand. Physical dependence means your body needs the drug to feel “normal” and maintain homeostasis, its internal balance. Addiction, on the other hand, involves compulsive drug-seeking behavior despite harmful consequences.
Your brain plays a starring role in this drama. Drugs hijack the brain’s reward system, particularly by flooding it with neurotransmitters like dopamine, often called the “reward chemical.” With continuous drug use, the brain reduces its natural production of these chemicals and adjusts its receptors, becoming less sensitive to natural rewards. When the drug is removed, the brain struggles to create its own dopamine again, leading to a severe chemical imbalance. This is often referred to as a “dopamine rebound” effect, where the brain tries to compensate, causing intense discomfort and cravings.
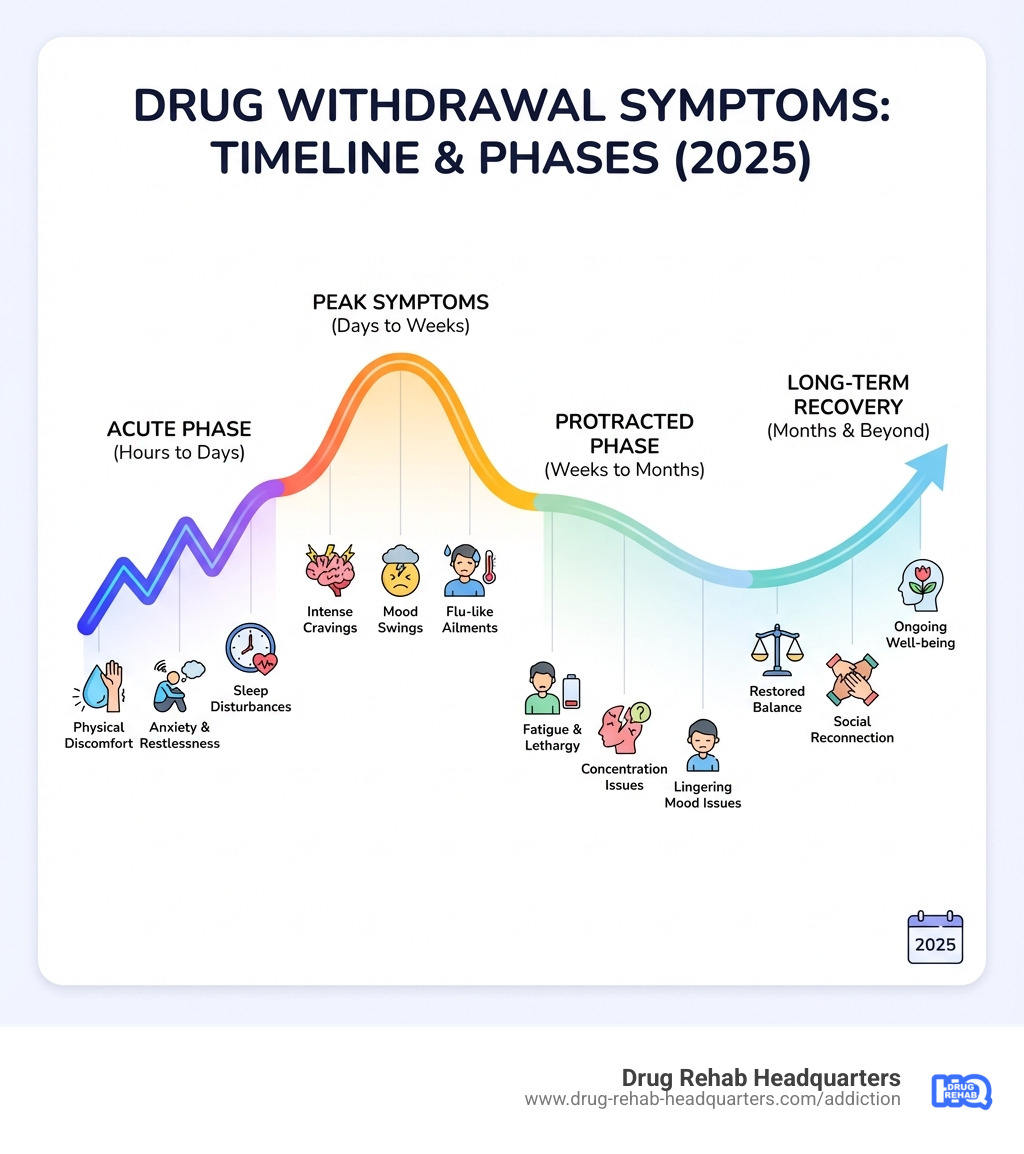
This physiological dance between the drug and your body leads to drug withdrawal symptoms. The severity and type of symptoms depend on many factors, but they generally fall into two phases:
- Acute Withdrawal: This is the initial phase, often the most intense, where physical symptoms are prominent. It’s when the substance starts to leave the body.
- Post-Acute Withdrawal Syndrome (PAWS): This phase can follow acute withdrawal and is characterized by less severe but persistent psychological and emotional symptoms that can last for weeks, months, or even years.
Beyond physical dependence, there’s also psychological dependence, where the mind craves the drug’s effects, often to cope with emotions or situations. Both types of dependence contribute to the challenging experience of withdrawal. Understanding these mechanisms helps us approach withdrawal with the compassion and medical expertise it requires. For more insight into the underlying processes, you can explore resources that explain the neurobiology of substance use.
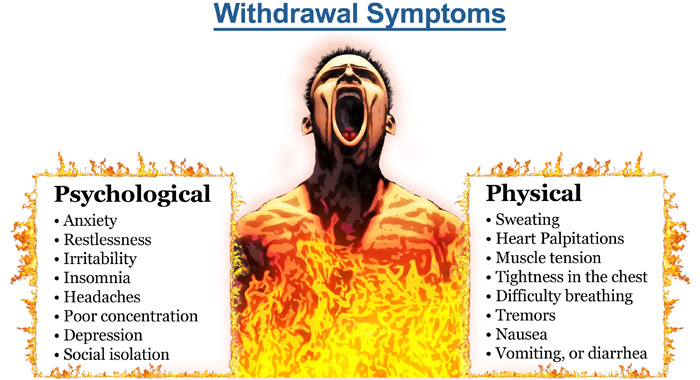
Recognizing Common Drug Withdrawal Symptoms and Potential Dangers
Recognizing the signs of drug withdrawal symptoms is the first step toward getting help. These symptoms can be incredibly varied, encompassing physical, psychological, and emotional distress. And while some are merely uncomfortable, others can be outright dangerous or even life-threatening.
The most common symptom across nearly all types of withdrawal is intense cravings. Your body and mind scream for the substance they’ve grown to depend on. Beyond cravings, the symptoms diverge significantly depending on the drug involved.
It’s vital to highlight that withdrawal from certain substances, particularly alcohol and benzodiazepines, can be extremely dangerous. Without proper medical supervision, individuals withdrawing from these drugs face severe risks, including seizures and a potentially fatal condition known as Delirium Tremens (DTs). DTs can manifest as severe confusion, hallucinations, rapid heartbeat, and fever. Other serious complications can include severe dehydration from vomiting and diarrhea, and cardiac complications due to the strain on the cardiovascular system. In some cases, the psychological distress and depression during withdrawal can lift the risk of suicidal thoughts.
General Physical Drug Withdrawal Symptoms
When your body is detoxing, it’s essentially in a state of shock, trying to recalibrate without the substance it’s used to. This often leads to a host of uncomfortable physical drug withdrawal symptoms:
- Nausea and vomiting: Your digestive system can go into overdrive or shut down, leading to severe stomach upset.
- Sweating and chills: Your body’s temperature regulation system can become erratic, causing you to swing between feeling freezing cold and drenched in sweat.
- Muscle aches and pains: It can feel like you’ve run a marathon you didn’t sign up for, with widespread body aches and muscle cramps.
- Headaches: Often throbbing and persistent, headaches are a common companion during withdrawal.
- Tremors or shaking: Involuntary shaking, especially in the hands, is a classic sign of withdrawal, particularly from alcohol and benzodiazepines.
- Fatigue: Paradoxically, despite restless nights, you might feel overwhelming exhaustion.
- Changes in appetite: You might lose your appetite entirely or experience intense hunger.
- Sleep problems (insomnia): Getting quality sleep can become a distant dream, leading to further physical and mental strain.
Common Psychological and Emotional Symptoms
The mind can be just as turbulent as the body during withdrawal. Psychological and emotional drug withdrawal symptoms can be particularly distressing:
- Anxiety and panic attacks: A pervasive sense of dread, nervousness, and sudden, overwhelming panic can take hold.
- Depression: A deep sadness, hopelessness, and lack of pleasure in activities you once enjoyed are common.
- Irritability and agitation: Small annoyances can feel like major provocations, leading to a short temper and restlessness.
- Mood swings: Your emotions might rollercoaster, shifting rapidly from euphoria to despair.
- Difficulty concentrating: Focusing on tasks, conversations, or even a simple TV show can become nearly impossible.
- Confusion or disorientation: Feeling foggy-headed, disoriented, or unsure of your surroundings can occur, especially in severe cases.
- Hallucinations: Seeing, hearing, or feeling things that aren’t there can be a terrifying experience, particularly with alcohol and benzodiazepine withdrawal.
- Paranoia: A feeling that others are out to get you or that something bad is about to happen can be unsettling.
These symptoms, both physical and psychological, underscore the critical need for professional medical supervision during withdrawal. Trying to tough it out alone is not only incredibly difficult but can also be dangerous.
Drug Withdrawal Timelines and Symptoms by Substance
The journey through withdrawal is highly individualized, but certain patterns emerge based on the substance involved. Factors influencing the timeline and severity include: the specific substance type, how long and how much of the drug was used (duration of use and dosage), and the individual’s overall health and metabolism. Generally, short-acting substances tend to have a quicker onset of withdrawal symptoms but may resolve faster, while long-acting substances might have a delayed onset but protracted symptoms.
Alcohol Withdrawal
Alcohol withdrawal is notorious for being one of the most dangerous withdrawal syndromes. Symptoms typically begin within 6-24 hours after the last drink, peak around 24-72 hours, and can last anywhere from 2-10 days. For more detailed insights, you can review our more info about alcohol detox.
Common symptoms include anxiety, shakiness, headaches, nausea, vomiting, sweating, and insomnia. However, the severe risks associated with alcohol withdrawal are what make medical supervision absolutely essential. These include:
- Seizures: Can occur within 12-48 hours after the last drink.
- Delirium Tremens (DTs): A severe and potentially fatal condition characterized by confusion, hallucinations, rapid heartbeat, and fever, usually appearing 48-72 hours after cessation.
An overview of alcohol withdrawal emphasizes the importance of medical attention due to its life-threatening potential.
Opioid (Heroin, Fentanyl, Painkillers) Withdrawal
Opioid withdrawal, while uncomfortable, is typically not life-threatening. However, the severe discomfort makes the relapse risk incredibly high.
- Short-acting opioids (e.g., heroin): Withdrawal symptoms generally begin 8-24 hours after last use and last an average of 4-10 days.
- Long-acting opioids (e.g., methadone): It may take 2-4 days for withdrawal symptoms to emerge. Withdrawal will likely fade within a period of 10-20 days.
Symptoms are often described as an intense flu-like illness, including: muscle cramps, bone pain, nausea, vomiting, diarrhea, sweating, runny nose, watery eyes, restless legs, yawning, and anxiety.
Benzodiazepine (Xanax, Valium) Withdrawal
Benzodiazepine (benzo) withdrawal is another category that carries significant risks, including seizures, making medical tapering crucial.
- Onset: Withdrawal may begin within 1-4 days after the last use.
- Peak: Symptoms typically peak in severity in the first 2 weeks.
- Duration: Withdrawal can last for weeks to months. In some cases, certain symptoms of protracted withdrawal can remain troublesome for months or years without treatment.
- Protracted Withdrawal Syndrome (PAWS): This is particularly common with benzodiazepines, where psychological symptoms like anxiety, insomnia, and cognitive difficulties can persist long after the acute phase.
Due to the high risk of seizures and the potential for protracted symptoms, benzodiazepine withdrawal should always be medically supervised. A gradual reduction of the dose over time is the safest approach.
Stimulant (Cocaine, Meth, Adderall) Withdrawal
Withdrawal from stimulants like cocaine, methamphetamine (meth), and prescription drugs like Adderall typically follows a different pattern, often characterized by a “crash” rather than severe physical danger.
- Onset: Symptoms begin within 24 hours of last use.
- Duration: Symptoms generally last for 3-5 days.
Common symptoms include:
- “Crash”: Extreme fatigue, excessive sleep, and intense hunger.
- Severe depression: Often accompanied by anhedonia (inability to feel pleasure) and sometimes suicidal thoughts.
- Intense cravings: A powerful urge to use the drug again.
- Agitation and irritability: Feeling restless and easily frustrated.
- Paranoia: Especially with meth withdrawal, psychotic symptoms can emerge.
While generally not life-threatening like alcohol or benzo withdrawal, stimulant withdrawal can be incredibly uncomfortable and psychologically challenging, leading to a high risk of relapse. For more information on specific stimulant withdrawals, you can refer to our guide to Adderall withdrawal and our guide to Meth withdrawal.
Navigating Recovery: Treatment and Management of Withdrawal
Starting on the path to recovery often starts with navigating the turbulent waters of withdrawal. It’s a challenging but necessary first step, and it’s one that no one should face alone. The importance of medical supervision during this period cannot be overstated. As we’ve seen, some withdrawal syndromes can be dangerous, even fatal, without professional care.
Detoxification (detox) is the process of safely eliminating drugs from the body while managing drug withdrawal symptoms. This process can occur in various settings:
- Inpatient settings: These facilities provide 24/7 medical supervision and support, which is ideal for severe withdrawal or for individuals with co-occurring medical or mental health conditions.
- Outpatient settings: For milder cases, outpatient detox allows individuals to live at home while attending regular medical appointments and receiving medication.
The choice between inpatient and outpatient detox depends on the severity of symptoms, the type of substance, an individual’s medical history, and their home support system. A medical team will assess these factors to determine the safest and most effective approach.
Struggling with withdrawal is difficult and can be dangerous. Call our 24/7 confidential helpline at 866-720-3784 to find a safe detox program near you. Whether you’re in Las Vegas, Reno, Henderson, or any of our other locations across the country, we can connect you with appropriate care.
The Role of Medication in Managing Drug Withdrawal Symptoms
Medication plays a crucial role in making withdrawal safer and more comfortable. This approach, often called Medication-Assisted Treatment (MAT), uses FDA-approved medications in combination with counseling and behavioral therapies.
Here’s how medication can help manage drug withdrawal symptoms:
- Buprenorphine (Suboxone): Often combined with naloxone, buprenorphine is used to treat opioid withdrawal and can shorten the length of detox. It helps alleviate withdrawal symptoms and reduce cravings by acting as a partial opioid agonist.
- Methadone: Another opioid agonist, methadone relieves opioid withdrawal symptoms and is also used for long-term opioid dependence maintenance, with doses slowly decreased over time.
- Naltrexone: This medication helps prevent relapse by blocking the euphoric effects of opioids and reducing alcohol cravings. It’s important that Naltrexone is only administered after detox is complete and the individual is opioid-free, as it can precipitate severe withdrawal if opioids are still in the system.
- Benzodiazepines for alcohol withdrawal: Medications like diazepam or lorazepam are the drugs of choice for managing acute alcohol withdrawal. They help prevent seizures and reduce agitation and anxiety.
- Clonidine for physical symptoms: This medication can help reduce many physical drug withdrawal symptoms such as anxiety, agitation, muscle aches, sweating, and runny nose, particularly in opioid withdrawal. However, it does not address cravings.
- Symptomatic medications: These are used to address specific uncomfortable symptoms, such as anti-nausea medications for vomiting, anti-diarrhea medications, and sleep aids for insomnia.
The use of these medications is guided by clinical expertise and often follows established clinical guidelines for withdrawal management.
Non-Medical Treatments and Finding Help
While medical supervision is paramount during acute withdrawal, non-medical treatments and ongoing support are essential for long-term recovery. These approaches help address the psychological and emotional facets of addiction and provide coping mechanisms.
Here’s a list of non-medical support options:
- Individual therapy (CBT): Cognitive-behavioral therapy (CBT) helps individuals identify and change negative thought patterns and behaviors that contribute to substance use.
- Group counseling: Sharing experiences and strategies in a supportive group setting can reduce feelings of isolation and provide encouragement.
- Holistic therapies: Practices like yoga, meditation, and guided imagery can help manage stress, improve mental well-being, and promote relaxation. Nutritional counseling also plays a role in restoring physical health.
- Support groups: Organizations like SMART Recovery and 12-Step programs (e.g., Alcoholics Anonymous, Narcotics Anonymous) offer peer support and a structured path to sobriety.
- Finding treatment centers: Our team at Drug Rehab Headquarters can assist you in finding reputable treatment centers across our network of locations, from Los Angeles to New York City, Houston to Chicago, and specifically in Nevada cities like Las Vegas, Reno, and Henderson. We can help you explore your options for drug withdrawal treatment that fit your individual needs.
These non-medical approaches, often integrated into comprehensive treatment plans, are crucial for building a foundation for sustained recovery after the acute phase of withdrawal has passed.
Life After Withdrawal: Long-Term Effects and Supporting a Loved One
Completing the initial detox and managing acute drug withdrawal symptoms is a monumental achievement, but it’s often just the beginning of a longer journey. Life after withdrawal involves addressing potential long-term effects and building a robust support system.
One significant long-term challenge is Post-Acute Withdrawal Syndrome (PAWS). Even after acute physical symptoms subside, psychological and emotional symptoms can linger for weeks, months, or even years. These might include mood swings, anxiety, depression, difficulty concentrating, sleep disturbances, and anhedonia. These symptoms fluctuate, sometimes intensely, making recovery feel like a rollercoaster.
Lingering cravings can also be a persistent challenge, requiring ongoing coping strategies and support. Many individuals also find or uncover co-occurring mental health disorders during or after withdrawal, such as depression, anxiety, or PTSD, which may have been masked or exacerbated by substance use. Treating these conditions concurrently is vital for sustained recovery.
Relapse prevention strategies become central to daily life, involving therapy, support group attendance, identifying triggers, and developing healthy coping mechanisms. Building a strong support network of family, friends, and peers in recovery is also incredibly important for navigating the ups and downs of sobriety.
How to Support Someone Going Through Withdrawal
Supporting a loved one through drug withdrawal symptoms can be incredibly challenging, both emotionally and practically. It’s like watching someone battle a severe illness, but one that often comes with stigma and misunderstanding. Here’s how you can help:
- Educate yourself: Understand what they’re going through, both physically and psychologically. Knowledge empowers empathy.
- Offer non-judgmental support: Avoid blaming or shaming. Your loved one needs compassion, not criticism.
- Encourage professional help: This is perhaps the most crucial step. Insist on medical supervision for detox, especially for alcohol and benzodiazepines. Offer to help them find a facility or make appointments.
- Help create a safe environment: Remove any substances from the home. Ensure they are in a calm, quiet space, free from stressors.
- Set healthy boundaries: While support is vital, enabling harmful behaviors is not. Protect your own well-being.
- Caregiver self-care: Supporting someone in withdrawal can be exhausting. Remember to eat well, get enough sleep, exercise, and lean on your own support system. You can’t pour from an empty cup.
Resources like the Alcohol and Drug Foundation offer valuable resources for family and friends navigating these difficult times. You don’t have to carry this burden alone. Our helpline at 866-720-3784 is also available 24/7 to provide guidance and connect you with family support resources.
Frequently Asked Questions about Drug Withdrawal
We understand that you might have many questions about drug withdrawal symptoms, and that’s perfectly normal. Here, we address some of the most common concerns.
How long do drug withdrawal symptoms last?
The duration of drug withdrawal symptoms varies significantly based on the type of drug, the length and intensity of its use, and individual factors like metabolism and overall health.
- Acute phase: This initial, most intense period typically lasts from a few days to a couple of weeks. For example, short-acting opioid withdrawal might last 4-10 days, while alcohol withdrawal typically runs 2-10 days.
- Post-acute withdrawal syndrome (PAWS): As discussed, psychological and emotional symptoms can linger much longer, potentially for months or even years. This is especially common with benzodiazepines, where symptoms can persist for months or years without proper treatment.
It’s a marathon, not a sprint, but with each passing day, the body heals and stabilizes.
Can you die from drug withdrawal?
Yes, unfortunately, withdrawal from certain substances can indeed be life-threatening without medical supervision.
- Alcohol withdrawal and benzodiazepine withdrawal pose the highest risks. The sudden cessation of these central nervous system depressants can lead to severe complications like seizures, Delirium Tremens (DTs), and cardiac arrest. These conditions can be fatal if not promptly and appropriately managed in a medical setting.
- While opioid withdrawal is uncomfortable and often described as feeling like a severe flu, it is generally not considered life-threatening in itself. However, the extreme discomfort can lead to dehydration and other complications, and the high risk of relapse after withdrawal, coupled with a decreased tolerance, significantly increases the risk of fatal overdose if drug use resumes.
This is precisely why we strongly advocate for medically supervised detox for anyone experiencing or anticipating drug withdrawal symptoms.
What helps with body aches from withdrawal?
Body aches, muscle cramps, and generalized discomfort are very common drug withdrawal symptoms, particularly with opioids and alcohol. Here’s what can help:
- Over-the-counter pain relievers: Medications like ibuprofen or acetaminophen can help manage mild to moderate aches. Always follow dosage instructions.
- Hot baths or showers: Warm water can help relax tense muscles and provide temporary relief from aches and chills.
- Gentle stretching or massage: Light stretching can ease muscle stiffness, and a gentle massage can improve circulation and reduce soreness.
- Staying hydrated: Dehydration can exacerbate muscle cramps and fatigue. Drinking plenty of water and electrolyte-rich fluids is crucial.
- Medically supervised detox: This is the most effective way to manage severe body aches and other withdrawal symptoms. Medical professionals can provide specific medications, such as clonidine for opioid withdrawal, which can significantly reduce physical discomfort and make the process much more tolerable.
Always consult with a healthcare professional before taking any new medications during withdrawal.
Conclusion: Your First Step Towards a New Beginning
Navigating drug withdrawal symptoms is undoubtedly one of the most challenging experiences a person can face. It’s a testament to the body’s incredible resilience and its struggle to find balance after prolonged substance use. From the intense physical discomforts like nausea and muscle aches to the profound psychological and emotional turmoil of anxiety and depression, withdrawal demands immense strength and support.
But here’s the most important takeaway: withdrawal is a manageable first step on the path to recovery. It is a temporary process, and with the right help, it can be done safely and effectively. We’ve explored how understanding the science behind dependence, recognizing the specific symptoms and timelines for different substances, and knowing the available medical and non-medical treatments can make all the difference.
At Drug Rehab Headquarters, we believe in the power of professional help and compassionate care. Our mission is to connect individuals across our locations, including cities like Las Vegas, Reno, and Henderson, with the resources they need to overcome addiction. Recovery is not just a dream; it’s a tangible reality that begins with taking that courageous first step.
You don’t have to steer this journey alone. We are here to guide you through every stage, from finding a safe detox program to connecting you with long-term support and therapy. Your new beginning is within reach.
Recovery is possible, and you don’t have to go through it alone.