Table of Contents
Understanding Percocet Abuse and Addiction
The Dangers of Percocet Misuse: Withdrawal and Overdose
Frequently Asked Questions about Percocet Addiction
Sustaining Sobriety: Aftercare and Long-Term Recovery
Comprehensive Percocet Addiction Treatment Options
Page Summary
Percocet addiction treatment is for people seeking help from Percocet addiction. Percocet is mostly known for the treatment of pain and its fever reducing qualities; however, it is also known as one of most addictive prescription medications. Like all prescription medications, people do not consider the long-term effects that may occur after using Percocet for a prolonged period of time. In fact, addiction to prescription medications, such as Percocet, is extremely powerful and can control every aspect of life.
Percocet Addiction Treatment involves a comprehensive approach to recovery that typically includes:
- Medical Detox: Safe withdrawal management under 24/7 supervision
- Medication-Assisted Treatment (MAT): FDA-approved medications like buprenorphine or methadone to reduce cravings
- Behavioral Therapy: Counseling approaches such as CBT and group therapy to address underlying issues
- Inpatient or Outpatient Rehab: Structured programs custom to addiction severity
- Aftercare Support: Ongoing therapy, support groups, and relapse prevention planning
Percocet Addiction Treatment starts with understanding what makes this medication so dangerous. Percocet combines oxycodone (a potent opioid) with acetaminophen (the active ingredient in Tylenol). Doctors prescribe it for moderate to severe pain, but what many people don’t realize is that it’s classified as a Schedule II controlled substance due to its high risk of abuse.
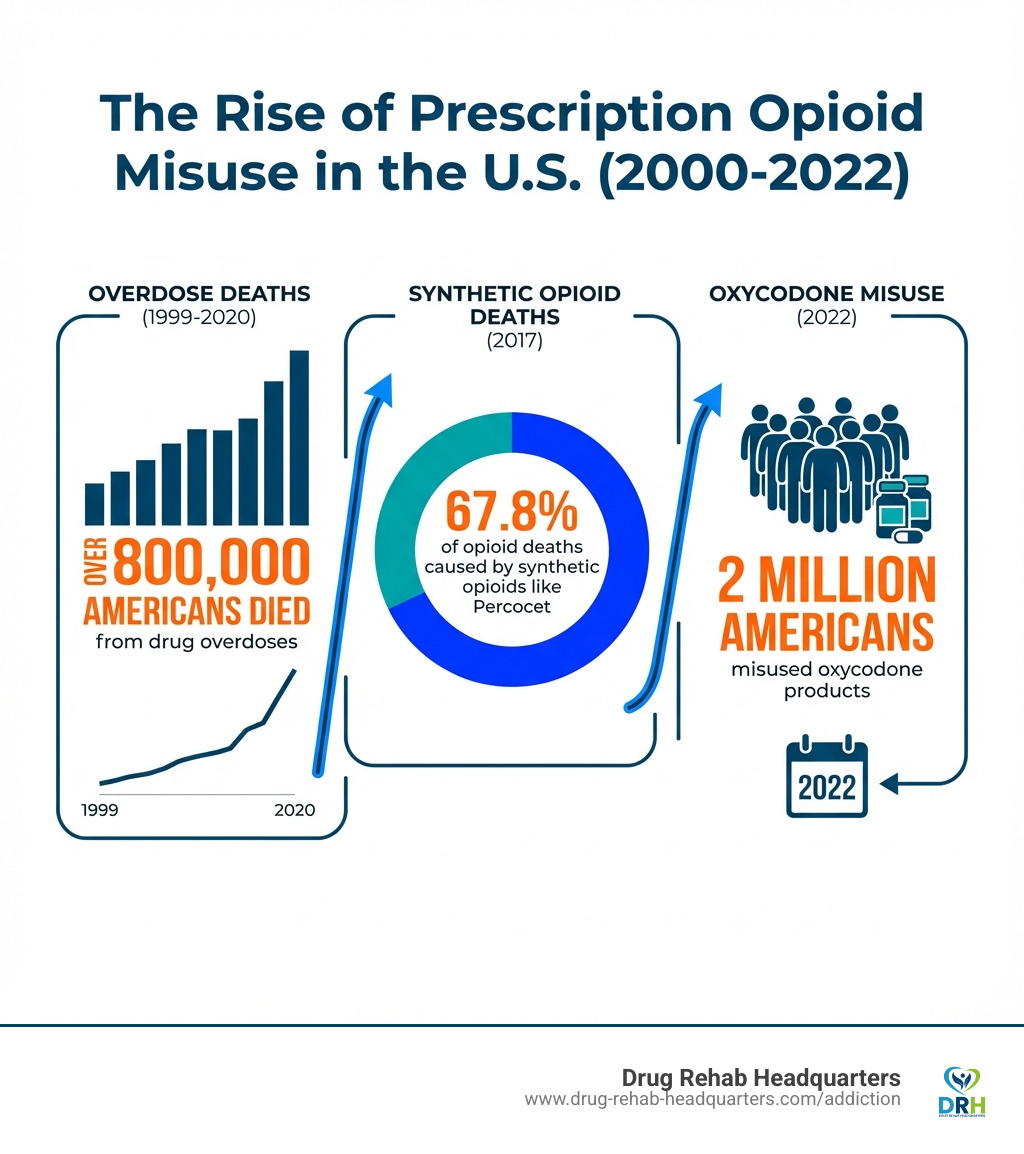
The numbers tell a sobering story. In 2022, more than 2 million Americans misused oxycodone products like Percocet. Since 2000, opioid-related deaths have increased by 300%. What often begins as legitimate pain management can quickly spiral into physical dependence and addiction—sometimes within just a week of prescribed use.
Physical dependence can develop even when taking Percocet exactly as prescribed. Your brain adapts to the drug’s presence, and stopping suddenly triggers uncomfortable withdrawal symptoms. For some people, the euphoria Percocet produces becomes a warning sign of vulnerability to addiction.
But here’s the crucial message: recovery is possible. Thousands of people successfully overcome Percocet addiction every year through evidence-based treatment programs.
At Drug Rehab Headquarters, we’ve helped countless individuals and families steer the path from Percocet addiction to lasting recovery, connecting them with comprehensive treatment options including medical detox, medication-assisted treatment, and ongoing support services. If you or a loved one is struggling, call us 24/7 at 866-720-3784 for a confidential assessment.
Understanding Percocet Abuse and Addiction
Percocet, a combination of the opioid oxycodone and acetaminophen, is a powerful pain reliever. While it can offer much-needed relief for acute, moderate to severe pain, its potent opioid component makes it highly addictive. Many individuals begin using Percocet with a legitimate prescription, only to find themselves developing a physical dependence and, eventually, an addiction. This slide from medical use to dependence can happen subtly, often unnoticed until the grip of addiction is firm.
Several factors can increase an individual’s risk of developing a Percocet addiction. Genetic predisposition plays a significant role; if addiction runs in your family, you may be more vulnerable. Environmental stressors, such as a chaotic home life, peer pressure, or easy access to the drug, can also contribute. Furthermore, co-occurring mental health disorders like depression, anxiety, PTSD, or bipolar disorder often go hand-in-hand with substance use disorders. People might initially use Percocet to self-medicate these underlying conditions, inadvertently fueling an addiction.
Recognizing the signs of Percocet abuse is the first critical step toward seeking help. These signs can manifest in various ways:
- Behavioral Changes: You might notice increased secretiveness, lying about drug use, “doctor shopping” (visiting multiple doctors to get more prescriptions), stealing pills, or asking for money more frequently. There’s often a preoccupation with obtaining and using the medication, sometimes leading to missed work, school, or social obligations.
- Physical Symptoms: Common physical indicators include chronic drowsiness, constricted (pinpoint) pupils, shallow or slowed breathing, frequent nodding off, and changes in sleep patterns (insomnia or sleeping too much). Other physical signs might include sweating, muscle and joint pain, or a general lack of coordination.
- Psychological Signs: Mood swings, increased irritability, heightened anxiety, or sudden bursts of anger are common. Individuals may become defensive when confronted about their drug use, often denying the problem despite clear evidence. Suspicion or paranoia can also develop.
If you observe these signs in yourself or a loved one, it’s crucial to understand that these are indicators of a serious problem. For more detailed information about the signs of opioid use disorder, you can refer to resources like this guide on opioid use disorder.
Short-Term and Long-Term Effects of Misuse
The effects of Percocet misuse can be immediate and severe, or they can accumulate over time, leading to devastating health consequences.
Short-term effects often include:
- Euphoria: A sense of intense pleasure or well-being, which is a major driver of misuse.
- Drowsiness and Sedation: Feeling unusually sleepy or “out of it.”
- Nausea and Vomiting: Common gastrointestinal disturbances.
- Constipation: A frequent and uncomfortable side effect of opioid use.
- Confusion and Dizziness: Impaired cognitive function and balance.
- Anxiety and Mood Swings: Emotional instability, even in the early stages of abuse.
However, the longer Percocet is misused, the more severe the consequences become. Long-term consequences can include:
- Liver Damage (from acetaminophen): The acetaminophen component in Percocet can cause serious liver damage at high doses, sometimes leading to acute liver failure, transplant, or death. This is independent of the opioid effects and can be particularly dangerous when individuals take more Percocet than prescribed.
- Kidney Failure: Chronic misuse places additional strain on the kidneys.
- Cardiovascular Problems: Opioid misuse can lead to heart-related issues, including an increased risk of heart attack or stroke.
- Brain Dysfunction: Long-term use can rewire the brain’s reward system, damaging the ability to feel pleasure from normal activities and leading to impaired cognitive function, memory loss, and difficulty making decisions.
- Respiratory Distress: Chronic shallow breathing can lead to sleep-disordered breathing and other lung complications.
- Hormonal Problems and Sexual Dysfunction: Opioids can disrupt hormonal balance, leading to issues like infertility.
- Weakened Immune System: Making individuals more susceptible to infections.
- Chronic Constipation and Bowel Obstruction: Severe and persistent gastrointestinal issues.
- Hallucinations: In some cases, prolonged high-dose use can lead to hallucinations.
For more information about the various side effects associated with Percocet, both short-term and long-term, you can explore resources like this page detailing side effects.
How Long Does Percocet Stay in Your System?
Understanding how long Percocet remains detectable in the body is important, especially for those considering Percocet Addiction Treatment or facing drug tests. Percocet’s effects typically last for about 4-6 hours, and its half-life (the time it takes for half of the drug to be eliminated from the body) is approximately 3.5 hours. While it leaves the bloodstream relatively quickly, its presence can be detected for varying periods depending on the type of test.

Here’s a general overview of detection windows:
- Urine Tests: Percocet metabolites can be detected in urine for up to two days after the last dose.
- Blood Tests: The drug can be found in the blood as fast as 15 minutes after a dose and may still be present up to 24 hours later.
- Saliva Tests: Typically, Percocet can be detected in saliva for 1 to 4 days.
- Hair Follicle Tests: These tests have the longest detection window, able to identify Percocet for up to 90 days.
Several factors influence how long Percocet stays in an individual’s system:
- Metabolism: People with faster metabolisms tend to eliminate drugs more quickly.
- Age: As we age, our bodies may process and eliminate substances more slowly.
- Dosage and Frequency of Use: Higher doses and more frequent use lead to longer detection times. Heavy, long-term abuse can also lead to accumulation in fatty tissue.
- Body Mass Index (BMI): Individuals with higher body fat percentages may store drugs for longer periods.
- Acetaminophen Presence: The acetaminophen in Percocet can put additional pressure on the liver, potentially affecting overall drug processing.
The Dangers of Percocet Misuse: Withdrawal and Overdose
Percocet misuse carries inherent dangers, but these risks escalate dramatically when combined with other substances. We cannot stress enough the extreme hazards of mixing Percocet with depressants like alcohol or benzodiazepines. This combination creates a synergistic effect, significantly increasing the risk of severe respiratory depression, which can be fatal. Both alcohol and benzodiazepines also depress the central nervous system, and when combined with the opioid oxycodone, they can slow breathing to dangerously low levels or even cause it to stop entirely.
Research consistently highlights the increased risks associated with polysubstance use. For a deeper dive into scientific research on polysubstance use, you can consult studies such as this one: scientific research on polysubstance use.
If you or someone you know is mixing Percocet with other substances, please understand the gravity of the situation. This is an emergency waiting to happen. For immediate help and guidance, please call us at 866-720-3784.
Percocet Withdrawal: Symptoms and Timeline
Once the body develops a physical dependence on Percocet, stopping its use can trigger a highly uncomfortable and challenging withdrawal process. It’s important to distinguish between physical dependence and addiction: physical dependence means the body has adapted to the drug and will experience withdrawal if it’s removed, while addiction involves compulsive drug-seeking behavior despite negative consequences. However, for Percocet, physical dependence often precedes addiction.
Withdrawal symptoms typically begin within 6-24 hours after the last dose, intensifying over the next few days. Common Percocet withdrawal symptoms include:
- Physical Discomfort: Intense muscle aches, bone pain, muscle twitches or tremors, profuse sweating, goosebumps (often called “cold turkey”), runny nose and watery eyes, yawning, and restless legs syndrome.
- Gastrointestinal Issues: Severe nausea, vomiting, abdominal cramps, and diarrhea.
- Psychological Distress: Agitation, anxiety, extreme irritability, dysphoria (a state of unease or generalized dissatisfaction), and intense cravings for Percocet.
- Sleep Disturbances: Insomnia, even when feeling exhausted.
The acute withdrawal timeline usually follows this pattern:
- First 72 hours: Symptoms often peak, resembling a severe flu. This is when physical discomfort and psychological distress are most intense.
- First week: While the peak subsides, many symptoms persist, gradually lessening in severity.
- Beyond a week (Post-Acute Withdrawal Syndrome – PAWS): For some individuals, lingering symptoms like sleep disturbances, mood problems, fatigue, and cravings can persist for weeks or even months. These gradually fade but require ongoing support.
Medical professionals often use tools like the Clinical Opiate Withdrawal Scale (COWS) to assess the severity of withdrawal symptoms and guide treatment. Attempting to manage Percocet withdrawal alone can be not only incredibly difficult but also dangerous, as the intense discomfort can lead to relapse.
Recognizing and Responding to a Percocet Overdose
A Percocet overdose is a life-threatening medical emergency requiring immediate action. It occurs when an individual takes too much of the drug, overwhelming the body’s systems, particularly the respiratory system.

Recognizing the signs of a Percocet overdose is critical:
- Severely Slowed or Stopped Breathing: This is the most dangerous sign. Breathing may be very shallow, gasping, or absent.
- Blue or Purple Fingernails or Lips: A clear indicator of lack of oxygen.
- Unresponsiveness: The person cannot be woken up, even with sternal rub or loud noises.
- Limp Muscles: The body appears very relaxed and floppy.
- Gurgling Sounds: Often described as a “death rattle.”
- Pinpoint Pupils: Pupils may be extremely small.
- Pale or Clammy Skin: Skin may feel cold and damp.
What to do in an emergency:
- Call 911 Immediately: This is the most important step. Provide your location and explain that someone is experiencing a potential opioid overdose.
- Administer Naloxone (Narcan) if Available: Naloxone is a medication that can rapidly reverse an opioid overdose. If you have it and know how to use it, administer it as directed. It will not harm someone who is not experiencing an opioid overdose.
- Stay with the Person: Keep them awake and breathing if possible. Position them on their side to prevent choking if they vomit.
- Perform Rescue Breathing/CPR if Necessary: If the person is not breathing, perform rescue breathing or CPR until emergency medical services arrive.
Every second counts in an overdose situation. Don’t hesitate to act. For more information on opioid overdose and how to respond, SAMHSA provides valuable resources: information on opioid overdose from SAMHSA.
Comprehensive Percocet Addiction Treatment Options
Overcoming Percocet addiction is a journey that requires professional support and a personalized approach. At Drug Rehab Headquarters, we understand that recovery is not a one-size-fits-all process. We are dedicated to helping individuals find the right continuum of care, custom to their unique needs and circumstances. Our extensive network includes top-rated facilities across numerous states, including Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming.
For example, if you’re looking for support in the Northeast, we can help you find a treatment center in Massachusetts. Or, if you’re on the West Coast, we’re ready to assist you in finding a treatment center in California, including major cities like Los Angeles, San Francisco, and San Diego. Our goal is to connect you with the best possible treatment options to begin your recovery journey.
The First Step: Medically Supervised Detox for Percocet Addiction Treatment
The first critical step in Percocet Addiction Treatment is often medically supervised detoxification. This is a period where the body is safely cleared of Percocet under the watchful eye of medical professionals.
The primary purposes of detox are:
- Managing Withdrawal Symptoms Safely: As we discussed, Percocet withdrawal can be incredibly uncomfortable and, in some cases, dangerous. Medical staff can administer medications to alleviate severe symptoms like nausea, vomiting, muscle aches, and anxiety, making the process more tolerable.
- 24/7 Medical Supervision: Round-the-clock care ensures that any complications, such as dehydration or severe psychological distress, are addressed immediately.
- Preventing Dangerous Complications: While opioid withdrawal is rarely life-threatening on its own, the intense discomfort can lead to dangerous behaviors or medical issues if unsupervised.
Detox alone is not a complete treatment for addiction. Research shows that most people who stop taking opioids without being stabilized on further treatment will quickly relapse, and this is extremely dangerous due to a rapid loss of tolerance. Detox is merely the first, albeit vital, step to stabilize an individual before they can engage in comprehensive therapy and long-term recovery strategies. To learn more about the process of prescription drug detox, we encourage you to read our detailed guide: learn more about prescription drug detox.
Medication-Assisted Treatment (MAT) for Opioid Use Disorder
Medication-Assisted Treatment (MAT) is an evidence-based approach that combines FDA-approved medications with counseling and behavioral therapies. It has proven highly effective in treating opioid use disorder, including Percocet addiction.
How MAT works:
- Reducing Cravings: Medications help normalize brain chemistry, significantly reducing the intense cravings that often lead to relapse.
- Preventing Relapse: By managing withdrawal symptoms and cravings, MAT allows individuals to focus on their recovery work in therapy.
- Improving Outcomes: Studies show that pharmacologic treatment for opioid use disorder reduces overdose mortality by nearly 50% and is associated with higher rates of treatment retention.
The FDA-approved medications used in MAT include:
- Buprenorphine (often combined with naloxone, marketed as Suboxone): This partial opioid agonist helps reduce withdrawal symptoms and cravings without producing the full euphoric effects of other opioids. Medical guidelines often recommend buprenorphine/naloxone as a first-line therapy due to its lower risk of overdose and fewer side effects compared to full opioid agonists. For more detailed information on buprenorphine/naloxone, you can consult guidelines such as those found here: Provincial guidelines on Buprenorphine/Naloxone.
- Methadone: A full opioid agonist that helps stabilize individuals and prevent withdrawal symptoms and cravings. Methadone treatment is typically administered in specialized Opioid Treatment Programs (OTPs).
- Naltrexone (marketed as Vivitrol in extended-release injectable form): This medication blocks opioid receptors, preventing opioids from producing their euphoric effects. It is non-addictive and can be a good option for individuals who have completed detox and are motivated to remain opioid-free.
MAT is most effective when integrated with comprehensive counseling and therapy, addressing both the physical and psychological aspects of addiction.
Inpatient vs. Outpatient Rehab Programs
Choosing the right level of care is a crucial decision in Percocet Addiction Treatment. We offer connections to both inpatient and outpatient programs, each designed to meet different needs.
| Feature | Inpatient Rehab | Outpatient Rehab |
|---|---|---|
| Environment | Structured, 24/7 supervised, residential setting | Flexible, allows living at home, scheduled sessions |
| Intensity | High, immersive, removes external triggers | Variable (IOP, PHP), allows daily responsibilities |
| Support | Constant medical & therapeutic support | Regular therapeutic support, less direct supervision |
| Ideal For | Severe addiction, co-occurring disorders, unstable home environment | Mild to moderate addiction, strong support system, work/school commitments |
| Duration | Typically 30, 60, or 90 days, sometimes longer | Varies, often longer-term, several hours/week |
Inpatient rehab offers a highly structured and supportive environment, away from the triggers and stresses of daily life. This 24/7 immersive experience is often ideal for individuals with severe Percocet addiction, those with co-occurring mental health disorders, or those who lack a stable and sober home environment. It allows for intensive therapy, medical monitoring, and a focus solely on recovery. To explore various inpatient drug rehab programs, you can visit our page: explore inpatient drug rehab programs.
Outpatient rehab programs, including Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs), provide flexibility, allowing individuals to live at home while attending scheduled therapy sessions and groups. This option is suitable for those with mild to moderate addiction, a strong support system at home, or responsibilities like work or school that they need to maintain. It allows for a gradual reintegration into daily life while receiving ongoing support.
Behavioral Therapies in Percocet Addiction Treatment
While medical interventions like detox and MAT address the physical aspects of Percocet addiction, behavioral therapies are essential for tackling the psychological roots and learned behaviors associated with substance use. These therapies teach individuals new coping mechanisms and strategies for maintaining sobriety.
Key behavioral therapies include:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors that contribute to drug use. It teaches skills for coping with cravings, managing stress, and preventing relapse.
- Dialectical Behavior Therapy (DBT): A form of CBT that focuses on emotional regulation, mindfulness, distress tolerance, and interpersonal effectiveness. It’s particularly effective for individuals with co-occurring mental health disorders or difficulty managing intense emotions.
- Group Therapy: Provides a supportive environment where individuals can share experiences, receive feedback, and develop social skills in a sober setting. It fosters a sense of community and reduces feelings of isolation.
- Family Counseling: Addresses the impact of addiction on family dynamics and helps family members heal, improve communication, and establish healthy boundaries. It educates families on how to support their loved one’s recovery effectively.
These therapies equip individuals with the tools they need to understand their addiction, manage triggers, and build a fulfilling life in recovery. To find more about behavioral health programs and how they can support your journey, visit: discover behavioral health programs.
Treating Co-Occurring Disorders
It’s common for individuals struggling with Percocet addiction to also experience co-occurring mental health disorders, a condition often referred to as a “dual diagnosis.” These disorders can fuel each other, making effective treatment more complex.
Common co-occurring conditions include:
- Depression: Feelings of sadness, hopelessness, and loss of interest.
- Anxiety Disorders: Excessive worry, panic attacks, or social anxiety.
- Post-Traumatic Stress Disorder (PTSD): Resulting from exposure to a traumatic event.
- Bipolar Disorder: Characterized by extreme mood swings.
The importance of integrated treatment cannot be overstated. When mental health disorders and addiction are treated separately, the chances of relapse are significantly higher. Integrated treatment addresses both conditions simultaneously, recognizing their interconnectedness and developing a comprehensive plan that supports healing on all fronts. This holistic approach leads to more sustainable long-term recovery. If you or a loved one needs this specialized care, we can help you find a dual diagnosis treatment facility that offers integrated treatment.
Sustaining Sobriety: Aftercare and Long-Term Recovery
Achieving sobriety from Percocet addiction is a monumental accomplishment, but recovery is a lifelong journey, not a destination. Sustaining sobriety requires ongoing commitment, vigilance, and a robust aftercare plan. Our goal at Drug Rehab Headquarters is not just to help you get sober, but to help you build a fulfilling and lasting sober life.
Aftercare planning is crucial for preventing relapse and reinforcing the skills learned during initial treatment. This often includes:
- Sober Living Homes: These provide a transitional, supportive, and drug-free environment for individuals graduating from inpatient programs, helping them gradually reintegrate into society.
- Support Groups: Programs like Narcotics Anonymous (NA) offer peer support, shared experiences, and a structured path to recovery through the 12 Steps. These groups provide invaluable community and accountability.
- Continued Therapy: Regular individual or group counseling sessions help reinforce coping mechanisms, address new challenges, and process any underlying issues that may emerge in sobriety.
- Relapse Prevention Planning: Developing personalized strategies to identify and manage triggers, avoid high-risk situations, and quickly respond to cravings or urges.
The importance of aftercare programs cannot be overstated in maintaining long-term recovery. These programs provide the scaffolding needed to steer the complexities of life without returning to substance use. To learn more about aftercare options, visit our page on the importance of aftercare programs.
Building a strong support network, practicing self-care, and developing healthy coping mechanisms are also vital components of long-term sobriety. Recovery is an ongoing process of growth and self-findy. We are here to support you every step of the way. If you’re ready to discuss long-term recovery options and how we can connect you with the resources you need, please call us at 866-720-3784.
Frequently Asked Questions about Percocet Addiction
We understand that you may have many questions about Percocet addiction and its treatment. Here are some of the most common inquiries we receive:
How do I know if I have a Percocet addiction?
Recognizing Percocet addiction often involves a combination of behavioral, physical, and psychological signs. If you find yourself taking more Percocet than prescribed, experiencing intense cravings, making unsuccessful attempts to cut down or stop, neglecting responsibilities due to drug use, or continuing to use despite negative consequences in your life (e.g., job loss, relationship problems), these are strong indicators. Developing tolerance (needing more of the drug for the same effect) and experiencing withdrawal symptoms when you try to stop are also key signs of physical dependence, which is a hallmark of addiction. If you’re questioning your use, it’s a sign to seek a professional assessment.
Can you stop taking Percocet on your own?
Abruptly stopping Percocet, especially after prolonged or heavy use, is not recommended due to severe and potentially dangerous withdrawal symptoms. The intense discomfort of withdrawal can be overwhelming and often leads to relapse. Furthermore, the body’s rapid loss of tolerance during a period of abstinence means that if you do relapse, you’re at a much higher risk of overdose. A medically supervised detox is the safest and most effective way to quit Percocet, as medical professionals can manage withdrawal symptoms, ensure your comfort, and prevent complications.
How long does Percocet addiction treatment last?
The duration of Percocet Addiction Treatment varies significantly based on individual needs, the severity of the addiction, the presence of co-occurring disorders, and the type of program. Initial treatment programs, such as inpatient or residential rehab, typically last 30, 60, or 90 days. However, recovery is a lifelong process, and these initial programs are usually followed by ongoing aftercare, which can include outpatient therapy, support groups, and sober living arrangements for several months or even years. The longer an individual engages in some form of recovery support, the better their chances of long-term success.
Conclusion: Your Path to Recovery Starts Today
Percocet, while a powerful pain reliever, carries a significant risk of dependence and addiction, leading to devastating consequences for individuals and their families. From the subtle slide from prescription use to full-blown addiction, to the dangers of withdrawal and the life-threatening risk of overdose, the path of Percocet misuse is fraught with peril.
However, we want to emphasize a message of hope: recovery is not only possible, it is achievable. Thousands of individuals successfully reclaim their lives from Percocet addiction every year through comprehensive, evidence-based treatment. Whether it’s through medically supervised detox, Medication-Assisted Treatment, intensive therapies, or ongoing aftercare, there are proven pathways to healing.
Taking the first step is often the hardest, but it’s the most courageous choice you can make. If you or a loved one is struggling with Percocet addiction, please don’t wait. Our team at Drug Rehab Headquarters is here to provide a confidential assessment and connect you with the right treatment program custom to your needs, in one of the many states we serve across the USA.
Your path to recovery starts today. Call our 24/7 helpline at 866-720-3784 to find the right treatment program for you.
