
Understanding Medical Detox: The Critical First Step in Addiction Recovery
Medical detox programs are professionally supervised services that help individuals safely withdraw from drugs or alcohol while managing potentially dangerous symptoms. These programs provide 24/7 medical monitoring, medication-assisted treatment, and a structured environment to clear substances from the body.
Key Facts About Medical Detox Programs:
- What it is: The process of clearing toxic substances from the body under medical supervision
- Duration: Typically 5-7 days, though alcohol detox averages 2-8 days and opioid detox can last 0-120 days
- Who needs it: Anyone physically dependent on alcohol, benzodiazepines, opioids, or other substances
- Where it happens: Licensed facilities with 24/7 medical staff, including hospitals, specialized detox centers, and residential treatment facilities
- What comes after: Transition to inpatient rehab, outpatient programs, or other addiction treatment services
If you or someone you love is struggling with addiction, understanding medical detox is essential. Detoxification is not the same as addiction treatment—it’s the critical first step that stabilizes your body and prepares you for the real work of recovery. According to SAMHSA (the Substance Abuse and Mental Health Services Administration), detox involves three essential components: evaluation of your physical and mental health, stabilization through withdrawal, and fostering your entry into ongoing treatment.
Attempting to quit substances “cold turkey” without medical supervision can be dangerous and even deadly. Alcohol withdrawal can cause seizures and delirium tremens (DTs), while benzodiazepine withdrawal carries similar life-threatening risks. Even opioid withdrawal, though rarely fatal, causes severe discomfort that often leads to relapse without proper support.
The statistics are sobering: only about one-fifth of people discharged from hospitals after detox receive substance abuse treatment during that hospitalization. Without follow-up care, detox alone has a high rate of relapse. This is why medical detox programs focus not just on getting substances out of your system, but on connecting you to the comprehensive treatment you need for lasting recovery.
At Drug Rehab Headquarters, we’ve guided countless individuals and families through the journey from detox to recovery, helping them understand their Medical detox programs options and connect with the right level of care. Our experience shows that informed patients who understand the detox process are better prepared for long-term success.
What is Medical Detox and Why is it Crucial?
When we talk about “detox” in the context of addiction, we’re referring to medical detoxification—a specialized process designed to safely and comfortably manage the physical withdrawal symptoms that occur when someone stops using drugs or alcohol. It’s about clearing toxic substances from the body under the watchful eye of a licensed medical team, usually led by a physician and supported by nurses, clinical staff, and therapists. This isn’t your average juice cleanse; this is serious medicine.
The primary goal of medical detox programs is to stabilize an individual’s physical condition while minimizing the discomfort and danger associated with withdrawal. Think of it like a hospital emergency department visit for an acute flare-up of a chronic medical condition. It stabilizes the immediate crisis but doesn’t, by itself, change the long-term course of the illness.
Why is this medical supervision so crucial? Because attempting to quit substances “cold turkey” can be incredibly dangerous, even deadly. For instance, severe alcohol withdrawal can lead to life-threatening complications like seizures and delirium tremens (DTs). Similarly, benzodiazepine withdrawal can trigger severe agitation, anxiety, and dangerous seizures. Unsupervised withdrawal from these substances is a gamble with very high stakes. Even for opioids, while withdrawal isn’t typically fatal, the intense physical discomfort (flu-like symptoms, body aches, nausea, vomiting) can be so overwhelming that it often drives individuals back to substance use, leading to a high risk of relapse.
It’s vital to understand that detoxification is not the same as substance abuse treatment. While it’s an essential first step, it’s not a cure for addiction. As SAMHSA emphasizes, detoxification is a distinct process focused on managing acute intoxication and withdrawal. It’s the bridge that gets you from active substance use to a stable state where you can begin the deeper work of addressing the psychological, social, and behavioral issues underlying addiction. Without this crucial distinction, individuals might leave detox feeling physically better but ill-equipped to maintain long-term sobriety. In fact, statistics show that only about one-fifth of people discharged from hospitals after detox receive substance abuse treatment during that hospitalization, and only 15 percent of those admitted through an emergency room for detox go on to receive any substance abuse treatment. This lack of follow-up significantly contributes to high relapse rates.
SAMHSA defines detoxification as having three essential components:
- Evaluation: This initial phase involves a thorough assessment of a patient’s physical and mental health, including screening for co-occurring disorders, testing for substances, and reviewing their substance use history. This helps the medical team understand the individual’s unique needs and potential risks during withdrawal.
- Stabilization: During this phase, the focus is on assisting the patient through acute intoxication and withdrawal to achieve a medically stable, substance-free state. This often involves 24/7 medical monitoring, administration of medications to ease withdrawal symptoms, and providing a safe, supportive environment.
- Fostering Entry into Treatment: This is perhaps the most critical component for long-term success. It involves educating the patient about addiction, stressing the importance of continued care, and preparing them for entry into comprehensive substance abuse treatment. The goal is to create a seamless transition from detox to the next phase of recovery, preventing the “revolving door” phenomenon where individuals repeatedly detox without addressing the root causes of their addiction. As SAMHSA’s Treatment Improvement Protocol (TIP) 45 states, detoxification is not a substitute for treatment, and its success is often measured by the patient’s entry into and retention in subsequent treatment.
Who Needs Medical Detox? Identifying the Signs and Substances
If you’re wondering whether medical detox programs are necessary for you or a loved one, the key indicators often revolve around physical dependence, tolerance, and the onset of withdrawal symptoms when substance use stops or is reduced.
- Physical dependence means your body has adapted to the presence of a substance and requires it to function “normally.”
- Tolerance means you need increasingly larger amounts of the substance to achieve the same effects.
- Withdrawal symptoms are the physical and psychological reactions that occur when the substance is removed from your system. These symptoms can range from uncomfortable to life-threatening.
Medical detox is necessary when there’s a risk of moderate to severe withdrawal symptoms. This is particularly true for substances that profoundly alter brain chemistry and bodily functions.
Here are some of the substances that most commonly require medically assisted detox and why:
- Alcohol: Alcohol withdrawal can be one of the most dangerous. Symptoms can appear within a few hours after the last drink and may include anxiety, tremors, nausea, vomiting, headache, insomnia, and rapid heartbeat. The most severe form is Delirium Tremens (DTs), which occurs in about five percent of alcohol withdrawal cases. DTs involve severe confusion, agitation, hallucinations, and seizures, and can be fatal without medical intervention. People with a history of seizures or previous DTs are at higher risk. You can learn more about the symptoms of alcohol withdrawal to understand the severity.
- Benzodiazepines (e.g., Xanax, Valium, Klonopin): These central nervous system depressants are often prescribed for anxiety, seizures, or sleep problems. Regular use, even for just six to eight weeks, can lead to physical dependence. Withdrawal can be extremely dangerous, mimicking alcohol withdrawal with symptoms like severe anxiety, agitation, tremors, rapid heart rate, and potentially fatal seizures. This is because the brain works harder to produce excitatory neurotransmitters to compensate for the drug’s depressive effects, and when the drug is suddenly removed, this overactivity can lead to dangerous neurological events.
- Opioids (e.g., heroin, fentanyl, OxyContin, Vicodin): While opioid withdrawal is rarely fatal on its own, it is notoriously uncomfortable. Symptoms can feel like a severe flu: cold and clammy skin, muscle aches, anxiety, nausea, vomiting, diarrhea, and intense cravings. The discomfort is so extreme that many individuals relapse to escape it, making medical supervision crucial for managing symptoms and preventing relapse. Physical dependence can develop in as little as six to eight weeks with regular, frequent use.
- Prescription Drugs (other than benzos/opioids): This category includes muscle relaxants, sleeping medications, and gabapentin. When misused or abused, these can also lead to significant physical dependence and withdrawal syndromes similar to alcohol and benzodiazepines, necessitating medical supervision for safe withdrawal.
- Stimulants (e.g., cocaine, methamphetamine, Adderall, Ritalin): Withdrawal from stimulants is primarily psychological, not life-threatening. Symptoms often include intense cravings, severe depression, fatigue, anxiety, and an inability to experience pleasure. The risk of relapse is very high due to the profound psychological discomfort and depressive symptoms, which can make medical detox important for managing these feelings and preventing immediate relapse, even though there isn’t a specific medication-assisted treatment (MAT) for stimulant withdrawal.
- Synthetic Drugs (e.g., “bath salts,” synthetic cannabinoids): The withdrawal experiences from these substances can be highly unpredictable and severe due to their varied and potent chemical compositions. Medical detox is essential to manage the unknown and potentially dangerous symptoms that may arise.
In summary, if a substance has created a physical dependence, and stopping its use could lead to uncomfortable or life-threatening withdrawal symptoms, medical detox programs are not just recommended, they are often a necessity for safety and to lay the groundwork for successful long-term recovery.
The Process of Medical Detox Programs: What to Expect

Entering a medical detox program can feel like a big step, but understanding the process can help ease any anxieties. Our goal at Drug Rehab Headquarters is to ensure you know exactly what to expect in a safe and supportive environment. The overall process is individualized, meaning it’s custom to your unique needs, medical history, and substance use patterns. However, there’s a typical flow that most individuals experience: admission, comprehensive assessment, stabilization, and discharge planning.
The Three Core Components of Detoxification
As outlined by SAMHSA, effective detoxification programs are built on three fundamental pillars:
-
Evaluation: This is where your journey in a medical detox program begins. Upon admission, a medical team will conduct a thorough and compassionate evaluation. This includes:
- Medical history review: Discussing your past and present health conditions.
- Substance use screening: Understanding the types of substances used, duration, frequency, and typical amounts.
- Co-occurring disorders assessment: Screening for any underlying mental health conditions (like anxiety or depression) that often accompany substance use disorders.
- Blood tests and other diagnostic checks: These help identify any immediate health risks, assess organ function, and confirm the presence of substances in your system.
This comprehensive evaluation allows the medical team to create a personalized treatment plan that addresses all your needs and anticipates potential withdrawal complications.
-
Stabilization: This is the core of the detox process, where your body physically clears the substances. It’s a critical phase where patient safety and comfort are paramount. You can expect:
- 24/7 medical monitoring: Nurses and physicians will closely track your vital signs (heart rate, blood pressure, temperature, breathing) around the clock.
- Symptom management: Medications are administered as needed to alleviate withdrawal symptoms, reduce cravings, and prevent severe complications.
- Safe and supportive environment: You’ll be in a controlled setting, free from the triggers and temptations of your usual environment, allowing you to focus solely on your physical recovery. Many facilities offer individual and group counseling during this phase to provide emotional support and begin addressing the psychological aspects of addiction.
-
Fostering Entry into Treatment: Detox alone is rarely enough for lasting recovery. This final component ensures you’re prepared for the next steps. It involves:
- Creating a continuing care plan: Working with counselors to develop a personalized plan for ongoing treatment, whether it’s inpatient rehab, outpatient programs, or other forms of therapy.
- Patient education on addiction: Helping you understand addiction as a chronic disease that requires ongoing management, much like diabetes or asthma.
- Preparing for rehab: Providing information, resources, and often direct referrals to the next level of care, ensuring a smooth transition into comprehensive treatment.
Medications Used in Medical Detox Programs
Medications play a vital role in medical detox programs, not only to reduce discomfort but also to prevent dangerous complications. The purpose of medication during detox is three-fold: to reduce cravings, manage withdrawal symptoms, and prevent severe, potentially life-threatening complications. Our understanding of addiction as a brain disease informs how these medications are used to help stabilize brain chemistry.
Here are some common medications used for specific types of detox:
- Alcohol Detox Medications: Benzodiazepines (like Librium or Valium) are frequently used to prevent seizures and delirium tremens, calm agitation, and reduce anxiety. Other medications may be used to address specific symptoms like nausea or sleep disturbances.
- Opioid Detox Medications:
- Buprenorphine (often in combination with Naloxone as Suboxone): This medication helps reduce opioid cravings and withdrawal symptoms without producing the same “high” as other opioids. It’s often used for medically assisted detox and long-term maintenance.
- Methadone: A long-acting opioid agonist, methadone has been used to prevent opioid withdrawal since the 1950s. It’s highly regulated and typically administered in specialized opioid treatment programs (OTPs).
- Naltrexone (oral or injectable Vivitrol): This medication blocks opioid receptors, preventing the euphoric effects of opioids and reducing cravings. It’s used after detox is complete to prevent relapse but can precipitate severe withdrawal if opioids are still in the system.
- Benzodiazepine Detox Medications: Benzodiazepines themselves are often used, but in a carefully controlled, tapering schedule, switching to a longer-acting benzodiazepine to gradually reduce the dosage over time. This slow reduction is critical to prevent seizures and other severe withdrawal symptoms.
How Long Does Medical Detox Last?
The question of “how long does medical detox last?” is a common one, and the answer, like much of addiction treatment, is: it depends. While medical detox programs typically last for five to seven days in most cases, this is an average. The duration is highly individualized and influenced by several factors:
- Substance type: Different substances have different withdrawal timelines. For example, alcohol withdrawal symptoms may level off within a week, with the average length of alcohol detox ranging from two to eight days. Opioid detox, depending on the specific opioid and method, can last much longer, sometimes from 0–120 days. Benzodiazepine withdrawal can be particularly protracted, sometimes requiring two weeks or longer for the acute phase.
- Duration of use: How long an individual has been using the substance plays a significant role. Longer periods of use often lead to more severe physical dependence and a more extended detox period.
- Amount used: The quantity of the substance consumed regularly directly impacts the intensity and duration of withdrawal. Higher doses generally mean a more challenging and potentially longer detox.
- Individual health: A person’s overall physical and mental health, including any co-occurring medical conditions (like heart disease or diabetes) or mental health disorders, can affect how their body processes withdrawal and how long stabilization takes.
- Co-occurring conditions: The presence of other health issues can complicate detox and require closer monitoring and potentially extended stays.
Our medical teams carefully monitor your progress and adjust your plan as needed, ensuring your safety and comfort throughout the entire process.
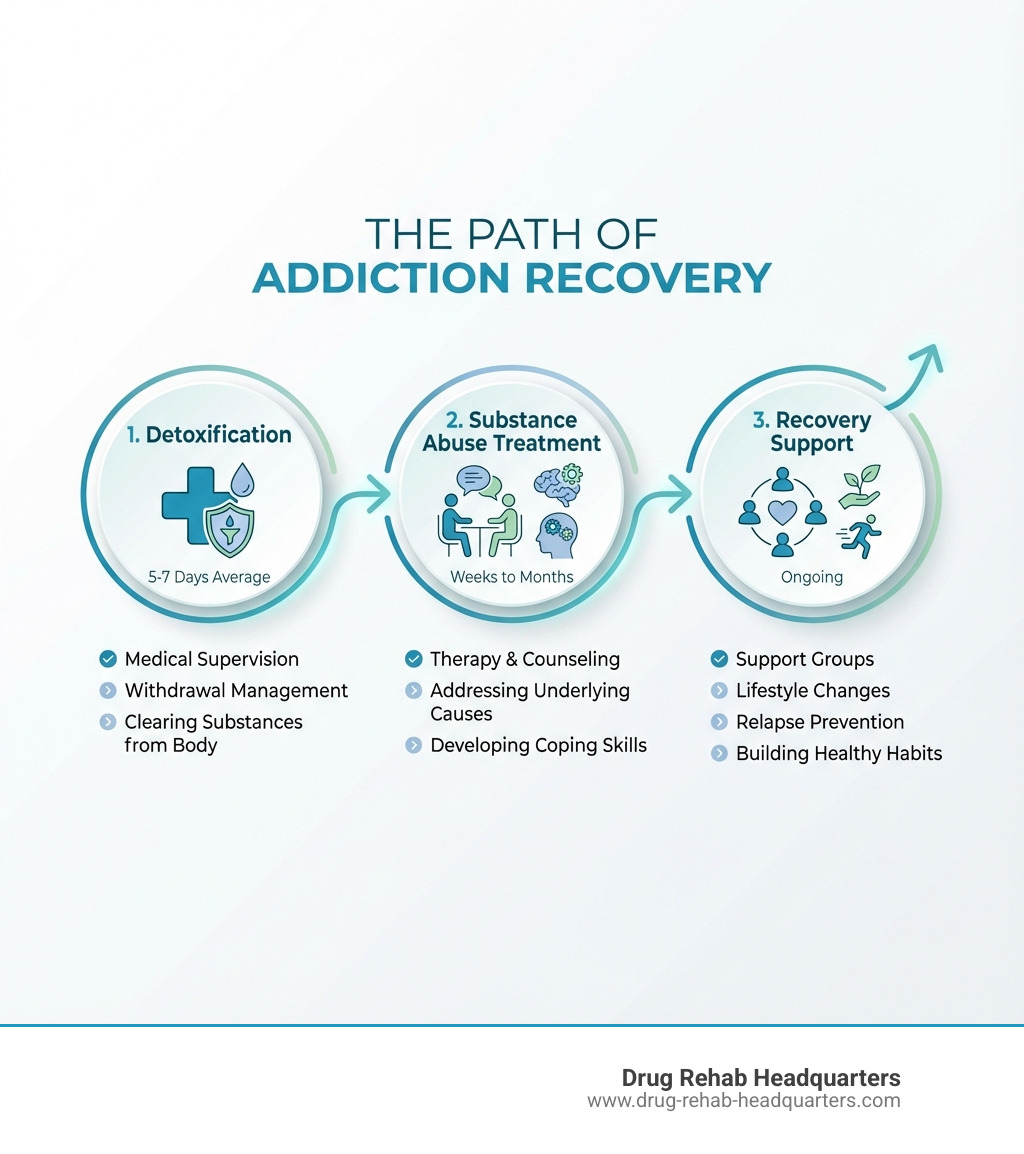
Life After Detox: The Path to Lasting Recovery
Successfully completing a medical detox program is a monumental achievement, a crucial first step on the path to recovery. However, detox is precisely that—a first step, not the entire journey. As we’ve discussed, detox addresses the physical dependence, but it doesn’t resolve the underlying psychological, emotional, and behavioral factors that contribute to addiction. Without follow-up treatment, there’s a high rate of relapse. Statistics show that only about 15 percent of people admitted to detox through an emergency room and then discharged receive any substance abuse treatment, highlighting a significant challenge in linking detox to ongoing care.
The real work of recovery begins after detox. This is where you learn to live a life free from substances, develop coping mechanisms, and address the root causes of your addiction. Our team at Drug Rehab Headquarters is dedicated to helping you steer these next steps.
Next Steps in Recovery:
- Inpatient Rehab: For many, transitioning directly into an inpatient or residential treatment program is the most effective next step. These programs provide a highly structured, supportive environment with 24/7 care, intensive therapy, and a focus on building new, healthy habits. They are particularly beneficial for individuals with severe addictions, co-occurring mental health disorders, or unstable home environments.
- Outpatient Programs (PHP, IOP): Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs) offer comprehensive therapy and support while allowing individuals to live at home or in sober living environments. PHPs typically involve several hours of treatment per day, multiple days a week, while IOPs offer a more flexible schedule.
- Individual Therapy: One-on-one counseling with a qualified therapist is essential for exploring personal triggers, past traumas, and developing personalized strategies for maintaining sobriety.
- Support Groups: Programs like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and other peer-led support groups provide invaluable community, shared experience, and ongoing encouragement.
- Medication-Assisted Treatment (MAT): For opioid and alcohol use disorders, MAT can be continued after detox to reduce cravings and prevent relapse, complementing therapy and counseling.
Finding a Reputable Program:
When looking for the next step in your recovery journey, it’s important to find a reputable program that aligns with your needs. Here’s what to look for:
- Licensing and Accreditation: Ensure the facility is licensed by the state and accredited by recognized organizations. This indicates they meet high standards of care.
- 24/7 Medical Staff: Even after detox, access to medical professionals is beneficial, especially in residential settings, to manage any lingering physical issues or co-occurring conditions.
- Evidence-Based Therapies: Look for programs that use proven therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and motivational interviewing.
- Comprehensive Care: A good program will offer a holistic approach, addressing not just substance use but also mental health, physical well-being, family dynamics, and aftercare planning.
Insurance Coverage:
Understanding your insurance coverage for addiction treatment, including medical detox programs, is crucial. Many insurance plans, including TRICARE, cover detoxification services. TRICARE, for example, covers the management of withdrawal symptoms for individuals with a substance use disorder, including inpatient services (emergency and non-emergency), intensive outpatient programs, partial hospitalization programs, and residential substance use disorder treatment in states like Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming.
Our team at Drug Rehab Headquarters can help you verify your benefits and understand what your insurance plan will cover, making the process of accessing care much smoother.
Frequently Asked Questions about Medical Detox
We understand you likely have many questions about medical detox programs. Here, we address some of the most common concerns to provide clarity and peace of mind.
Is medical detox a safe process?
Absolutely, yes. When supervised by a qualified medical team in a licensed facility, medical detox programs are designed to be a safe process. The primary purpose of medical detox is to prevent dangerous withdrawal complications and ensure your well-being. This safety is achieved through:
- 24/7 Medical Monitoring: Constant observation by nurses and doctors allows for immediate intervention if any complications arise.
- Medication Management: Specific medications are used to ease withdrawal symptoms, reduce discomfort, and prevent life-threatening events like seizures or delirium tremens.
- Licensed Facilities: Reputable medical detox centers adhere to strict safety protocols and are equipped to handle medical emergencies.
Attempting to detox alone significantly increases risk. With professional supervision, you are in the safest hands possible during this critical phase of recovery.
What are the most dangerous substances to detox from without medical help?
The substances that pose the greatest danger during unsupervised withdrawal are:
- Alcohol: Alcohol withdrawal can quickly escalate from uncomfortable to life-threatening. Symptoms can include severe tremors, hallucinations, and seizures. The most severe complication, delirium tremens (DTs), can be fatal due to cardiac arrest or respiratory failure if not medically managed.
- Benzodiazepines: Withdrawal from benzodiazepines (such as Xanax, Valium, Klonopin) is very similar to alcohol withdrawal in its severity and potential for danger. Abrupt cessation can lead to intense anxiety, psychosis, and severe, potentially fatal seizures.
For both alcohol and benzodiazepines, the risk of seizures and other life-threatening complications makes medical supervision an absolute necessity. Quitting “cold turkey” from these substances is never recommended.
Can I detox at home?
We strongly advise against attempting to detox at home, especially if you are physically dependent on substances like alcohol or benzodiazepines. While the idea of detoxing in the comfort of your own home might seem appealing, the risks far outweigh any perceived benefits.
- Extreme Danger for Certain Substances: As mentioned, alcohol and benzodiazepine withdrawal can cause seizures, DTs, and other severe medical emergencies that require immediate professional intervention. Without medical support, these situations can be deadly.
- High Risk of Relapse: Even for substances where withdrawal isn’t immediately life-threatening (like opioids), the intense discomfort and cravings can be overwhelming. Without professional support and medication to ease symptoms, the likelihood of relapsing to escape the pain is extremely high.
- Lack of Comprehensive Care: Home detox lacks the medical monitoring, medication management, and crucial connection to ongoing treatment that professional medical detox programs provide. It’s a temporary fix at best, and a dangerous gamble at worst.
Medical detox provides the safety, comfort, and foundation necessary to move forward into comprehensive addiction treatment. It’s an investment in your health and your future.
Conclusion: Your First Step Towards a Healthier Future
We hope this guide has demystified medical detox programs and highlighted their crucial role in the journey to lasting recovery. Addiction is a chronic condition, and medical detox is the essential first step—a safe and medically supervised process to clear substances from your body and manage withdrawal symptoms. It’s the bridge that stabilizes your physical health, preparing you for the deeper work of healing.
While detox is vital, it is not the destination. It’s the beginning of a transformative journey that requires ongoing commitment and comprehensive treatment. At Drug Rehab Headquarters, we understand that this journey can feel overwhelming, but you don’t have to walk it alone.
Our 24/7 free helpline is staffed by certified counselors, many with personal experience in recovery, who are ready to offer personalized guidance. We are here to help you understand your options, verify your insurance benefits, and connect you with evidence-based, holistic treatment options in states like Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming.
Your healthier future starts now. Let us help you take that courageous first step. Call our 24/7 helpline today to find a treatment program and begin your recovery journey.
